Mental health remains one of the most pressing yet under-addressed challenges globally, especially among young people. Across the African continent, millions of young people face stressors that deeply affect their mental well-being. To mark the world Mental Health Awareness Month, we sat down with Hildegarde Mukasakindi, Clinical Instructor at Partners In Health in Rwanda and a 2025 WomenLift Health East Africa Global Fellow, to unpack the state of mental health in Africa. Drawing from her work in community-based mental health care, Hildegarde shares timely insights on stigma, resilience, leadership, and how we can collectively create a healthier future.
- What are some of the primary drivers of mental health challenges among African youth today?
A 2021 study on mental health in Sub-Saharan Africa revealed that one in seven children and adolescents live with mental health problems, and one in ten meet the criteria for psychiatric diagnosis. Further, the prevalence of mental health challenges in adolescents affected by HIV/AIDS, exposure to violence, and poverty stands at 29% for depression, 19.3% for anxiety, 27% for post-traumatic stress (PTS), and 11.6% for suicidality.
Young people who are socio-economically vulnerable—like those experiencing poverty, inadequate access to basic needs, unemployment, exposure to violence and conflict, and orphanhood—are more susceptible to mental health problems. Other vulnerabilities like high social media usage, social pressures, conflict, alcohol and drug abuse, and inadequate access to supportive systems also raise vulnerability that if ignored could develop into mental health challenges.
- How have health emergencies such as the COVID-19 pandemic and the climate crisis impacted mental health across the continent?
COVID-19 brought about mass psychological distress, with high rates of mental health challenges including increased anxiety, depression, and insomnia reported during the pandemic. This was not only due to the loss of loved ones and increased economic hardship as a result of job losses, but also because of interventions such as quarantine, social distancing and isolation, which were psychologically draining and exacerbated loneliness, uncertainty, and stress.
The climate crisis causes additional psychological stressors. Eco-anxiety is a chronic fear that aligns with environmental degradation and its impacts, affecting many Africans. Droughts, floods, desertification, and food deficits threaten livelihoods, displace communities, and deepen poverty. These environmental processes fuel uncertainty and despair, undermining resilience and dampening the desire to participate in climate adaptation activities.
Overall, the interconnection of infectious disease, climate change, and socio-economic status creates a cumulative driver of mental health challenges in Africa. Efforts to combat such effects must be multidisciplinary in nature—integrating mental health services and enhancing community resilience, access to basic resources, and support from governments and other stakeholders.
- How can we address stigma to encourage more open conversations around mental health and improve access to mental health services?
Reduction of stigma at the community level requires a multi-intervention strategy consisting of robust mental health policies, education, community engagement, quality mental health care and empowerment programs.
Skills training in areas such as maintaining health following a diagnosis of mental illness, identifying strengths and goal setting, planning personal recovery, enhancing social skills, confronting stigma and violence, and improving livelihoods can empower those living with mental health disorders.
In addition, the integration of mental health care into national health systems can help deliver support more seamlessly and make it less stigmatizing. If mental health treatment is included as a routine part of care, seeking help becomes normalized and the rights of individuals with mental disorders can be better protected.
Establishing a culture of open communication, increasing access to quality care, and empowering affected persons comprise the key measures towards reducing stigma and improving mental well-being in African societies.
- Based on your extensive experience in delivering community-based mental health services, how has mental health care in Africa evolved over the past decade?
The past 10 years have been a welcome movement towards more equitable access to mental health care through community-based approaches in Africa. While some African countries have endorsed and implemented policies and programs to integrate mental health into primary health care, challenges around effective implementation, limited resources, inadequate infrastructure and training among medical professionals, together with stigma, persist.
That said, commendable efforts have been made to develop community-based, culturally appropriate, sustainable, cost-effective, and scalable interventions across Africa.
In Rwanda, for example, the Mentorship and Enhanced Supervision at Health Centers for Mental Health (MESH-MH) program, a collaboration between the Ministry of Health and Partners In Health, is aimed at strengthening primary health care by providing treatment of severe and common mental illnesses through community-based care, as per Rwanda’s National Mental Health Policy.
In Ethiopia, an integrated district-level model of delivering mental health care utilizing task-sharing has effectively filled the treatment gap in addressing severe mental disorders in rural environments. In Ghana, Positive Psychology Interventions (PPIs) have been successful implemented in rural settings. In Zimbabwe, psychological intervention with peer support is provided through the Friendship Bench program in rural settings to combat depression.
These are examples of community-level interventions with promising results and effectiveness in meeting mental health needs and yielding positive health outcomes. Scaling up these programs to aid in closing the treatment gap for mental disorders in Africa would make a significant difference to expanding and strengthening mental health care.
- Africa is home to six of the top ten countries with the highest suicide rates in the world. As a leader in global health, what role do you believe leadership plays in addressing the challenges around mental health in Africa?
Suicide is a critical public health issue that warrants urgent attention. Every 40 seconds someone takes his or her own life, and at least 90% of suicide victims are thought to suffer from a mental disorder, with approximately 60% of them being depressed at the time of death.
Young adults and adolescents aged 15 to 30 years are a high-risk group for suicide, which results from the interaction between biological, genetic, psychological, sociological, cultural, and environmental factors, as well as untreated mental health conditions.
Bold, inclusive, and transformative leadership is required to address the rising suicide rates across Africa. Such leadership should reinforce comprehensive policy reforms that place mental health within the overall agenda of public health, with adequate financing, resource mobilization, and the establishment of culturally appropriate, context-specific mental health services.
In addition, inclusive leadership should involve multiple stakeholders— community leaders, youth, women, and even traditional healers—to tackle the stigma around mental health. Mainstreaming mental health conversations and practice into everyday life fosters trust and ownership by the community. The participatory approach also creates supportive mechanisms that include family, friends, religious groups, community associations, and social networks. Enabling constructive engagement reinforces community resilience and mental well-being.
While such support networks can reduce suicidal risk, they cannot eliminate it. Transformational leadership must transcend ingrained systemic barriers, facilitate early recognition and treatment of mental health disorders, and advocate for the integration of mental health into the broader development agendas. It is also necessary to advocate for data-driven approaches to monitor progress and modify interventions accordingly.
- You are a strong advocate for community-based mental health care. Can you elaborate on the benefits of this approach and how it can be scaled up effectively?
Community-based mental health care enhances access to services, reduces stigma, improves medication adherence, prevents chronicity of illness, and is cost-effective, especially in low-income settings. They also limit long waiting times and lead to better health outcomes.
In addition, community-based mental health services promote culturally responsive and holistic approaches that enable individuals to receive services in comfortable, familiar environments. Engaging stakeholders from within communities enables frank discussions about mental health, which heightens awareness, acceptability, promotes early detection of mental illnesses, and reduces stigma. Facilitating the provision of care closer to patients’ homes also allows patients to remain close to their families, form meaningful relationships, avoid social isolation, and enhance community ownership and better health outcomes.
Scaling up mental health care in the community requires a multi-faceted approach to develop supportive national policies, build political will, engage communities and allocate funding, which are all critical steps. Prioritizing cost-effective interventions and leveraging data for ongoing improvement all contribute to sustainability of effective mental health care services.
Putting these measures in place can dramatically improve access, limit disparities, and improve mental health outcomes among populations.
- How can we better engage African youth in mental health advocacy and empower them to be part of the solution?
Integrating mental health education into school curricula and youth programs can increase awareness, enhance knowledge, and promote early help seeking to boost resilience. Providing training and leadership opportunities enables young people to serve as peer educators and advocates, teaching them with a sense of ownership and responsibility.
In today’s digital world, leveraging technology—mobile applications, online support groups, social media—is key to engaging more youth and making mental health conversations more accessible and engaging.
Including the youth as partners in policymaking and program design will also ensure their needs and concerns are heard, resulting in more effective interventions. Through education, youth-friendly forums, and participatory engagement, we can empower the youth to amplify mental health awareness and advocacy and influence systems of care in Africa.
- Looking ahead, what are your hopes and aspirations for the future of mental health care in Africa, and what steps do you believe are crucial to achieving these goals?
My hope is that mental well-being becomes an integral part of daily life for everyone at every stage of life. Just as we promote exercise and nutrition to improve physical health, we need to foster a culture of mental wellness by empowering individuals from a young age to thrive in spite of adversity and build resilience.
I call for leadership with a ripple effect—policy informing, resource organizing, and community stimulating toward a shared vision of improved mental health resilience and well-being in Africa.
Hildegarde Mukasakindi is a Clinical Instructor for the Mental Health Program at Partners In Health (Rwanda) and a 2025 WomenLift Health global Fellow









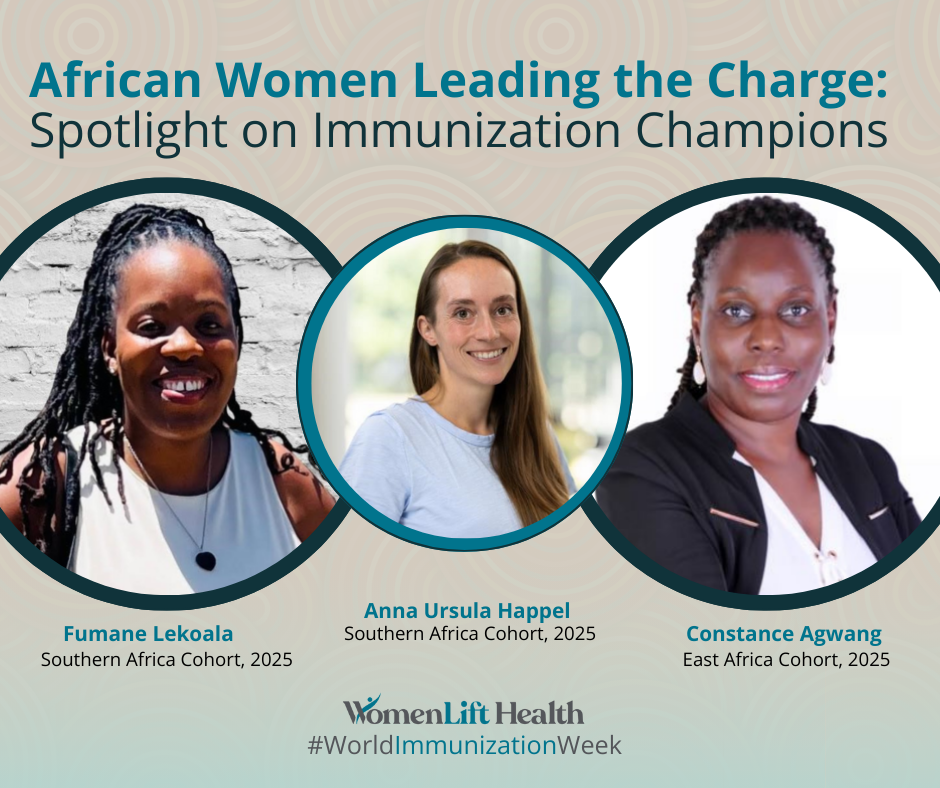
 Anna: Being a woman scientist working in immunization in Africa today means using research to drive real-world impact, especially for infants, who are among the most vulnerable. My work focuses on improving vaccine responses in early life, and it’s incredibly rewarding to contribute to solutions that give children a healthier start. It also means advocating for equity in science and helping pave the way for more women to lead in Public Health.
Anna: Being a woman scientist working in immunization in Africa today means using research to drive real-world impact, especially for infants, who are among the most vulnerable. My work focuses on improving vaccine responses in early life, and it’s incredibly rewarding to contribute to solutions that give children a healthier start. It also means advocating for equity in science and helping pave the way for more women to lead in Public Health. Fumane: Being a woman working in immunization in Africa today is both deeply rewarding and profoundly challenging. It means being at the forefront of community transformation, ensuring health equity, and advocating tirelessly to protect our future generations from preventable diseases. It’s about navigating complex health systems, building trust in communities, and continuously championing gender-inclusive leadership despite persistent barriers.
Fumane: Being a woman working in immunization in Africa today is both deeply rewarding and profoundly challenging. It means being at the forefront of community transformation, ensuring health equity, and advocating tirelessly to protect our future generations from preventable diseases. It’s about navigating complex health systems, building trust in communities, and continuously championing gender-inclusive leadership despite persistent barriers. Constance: Working in Immunization in Africa means resilience. Women in immunization in Africa face discrimination and security challenges, often limiting their ability to reach remote or conflict-stricken communities. There’s also a persistent marginalization of women from decision-making spaces, which negatively impacts health outcomes. Health systems perform better when women, who deliver much of the care, have an equal say in their design and delivery.
Constance: Working in Immunization in Africa means resilience. Women in immunization in Africa face discrimination and security challenges, often limiting their ability to reach remote or conflict-stricken communities. There’s also a persistent marginalization of women from decision-making spaces, which negatively impacts health outcomes. Health systems perform better when women, who deliver much of the care, have an equal say in their design and delivery.

 My journey into clinical research wasn’t a straight path—it has been a mix of curiosity, resilience, and an unwavering belief that Africa is more than just a participant in global health—it’s a leader in the making. From my early days in clinical research, I started my career asking tough questions: Why are certain populations underrepresented in trials? Why do life-saving treatments take so long to reach Africa? These questions led me to incredible opportunities, and over time I’ve been able to bridge global expertise with local needs, driving clinical trial and innovation across the continent. It’s been a process of utter learning, unlearning, and making sure clinical trials in Africa are sustainable, equitable, and truly representative. Every day, I get to bring people together—sponsors, researchers, and policymakers—to rethink what’s possible.
My journey into clinical research wasn’t a straight path—it has been a mix of curiosity, resilience, and an unwavering belief that Africa is more than just a participant in global health—it’s a leader in the making. From my early days in clinical research, I started my career asking tough questions: Why are certain populations underrepresented in trials? Why do life-saving treatments take so long to reach Africa? These questions led me to incredible opportunities, and over time I’ve been able to bridge global expertise with local needs, driving clinical trial and innovation across the continent. It’s been a process of utter learning, unlearning, and making sure clinical trials in Africa are sustainable, equitable, and truly representative. Every day, I get to bring people together—sponsors, researchers, and policymakers—to rethink what’s possible.